COPD: systemic proteomic profiles in frequent and infrequent exacerbators
Patients with COPD can suffer acute episodes of exacerbation (AE) of their respiratory symptoms
This episodes negatively impact their health status and prognosis.
For reasons still unclear, some COPD patients are particularly prone to suffering frequent exacerbations (FE) while others are not (NFE).
AE can be triggered by viral and bacterial respiratory infections and are associated with lung microbiome changes and/or airway eosinophilic infiltration that can result in a dysregulated host immune response, leading to local and systemic inflammation.
Accordingly, we hypothesised that the plasma proteomic profile of FE patients is different from that of NFE and may share some characteristics with an actual episode of AE.
To explore these hypotheses, we used a complementary two-way quantitative proteomic approach that combines an unbiased label-free mass spectrometry-based method with a targeted immunoassay-based workflow to compare the plasma proteome of clinically stable COPD patients with and without FE.
As a reference, we also determined the proteomic profile observed during an actual episode of AE and in healthy controls (HC).
Background
Some patients with COPD suffer frequent exacerbations (FE). We hypothesised that their systemic proteomic profile would be different from that of non-frequent exacerbators (NFE).
The objective of the present study was to contrast the systemic proteomic profile in FE versus NFE. As a reference, we also determined the systemic proteomic profile of healthy controls (HC) and COPD patients during an actual episode of exacerbation (AE).
Methods
In the analysis we included 40 clinically stable COPD patients (20 FE and 20 NFE), and 20 HC and 10 AE patients.
Their plasma samples were analysed by combining two complementary proteomic approaches: label-free liquid chromatography-tandem mass spectrometry and multiplex immunoassays.
Gene Ontology annotation, pathway enrichment and network analyses were used to investigate molecular pathways associated with differentially abundant proteins/peptides (DAPs).
Results
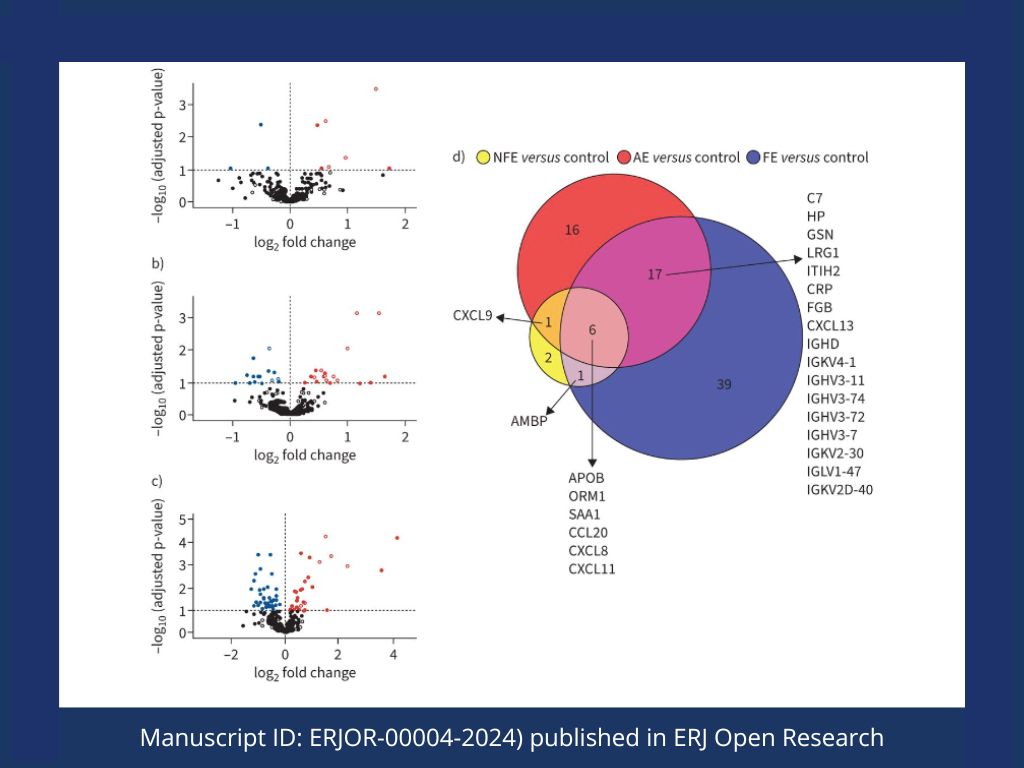
Compared with HC, we identified 40 DAPs in FE, 10 in NFE and 63 in AE.
Also compared to HC, pathway functional and protein–protein network analyses revealed dysregulation of inflammatory responses involving innate and antibody-mediated immunity in COPD, particularly in the FE group, as well as during an AE episode. Besides, we only identified alterations in the complement and coagulation cascades in AE.
Conclusion
There are specific plasma proteome profiles associated with FE, which are partially shared with findings observed during AE, albeit others are uniquely present during the actual episode of AE.
Authors
Cesar Jessé Enríquez-Rodríguez, Carme Casadevall, Rosa Faner, Ady Castro-Costa, Sergi Pascual-Guàrdia, Luis Seijó, José Luis López-Campos, Germán Peces-Barba, Eduard Monsó, Esther Barreiro, Borja G. Cosío, Alvar Agustí, Joaquim Gea, on behalf of the BIOMEPOC group.
Read more
Noticias relacionadas

Climate change and respiratory health: implications for respiratory clinicians in primary and specialist care
Review on climate change and respiratory health, focusing on chronic respiratory diseases and implications for primary and specialist care.
cfDNA profiling in COPD
Whole-genome cfDNA profiling identifies molecular clusters and pathways associated with oxidative damage and airflow limitation in COPD patients.

Video del evento: Transformando la EPOC, claves para un manejo proactivo
Conferencia sobre el manejo proactivo de la EPOC centrada en el infradiagnóstico, el control clínico y el seguimiento estructurado del paciente.
Artículos
EPOC
- 759788·Alvar Agustí, Rod Hughes, Eleni Rapsomaki, Barry Make, Ricardo Del Olmo, Alberto Papi, David Price, Laura Benton, Stefan Franzen, Jørgen Vestbo, Hana Mullerova – The many faces of COPD in real life: a longitudinal analysis of the NOVELTY cohort
- 759883·Alberto Papi, Rosa Faner, Ian Pavord, Federico Baraldi, Vanessa M McDonald, Mike Thomas, Marc Miravitlles, Nicholas Roche, Alvar Agustí. – From treatable traits to GETomics in airway disease: moving towards clinical practice
- 768778·Alvar Agusti, Claus F. Vogelmeier – GOLD 2024: a brief overview of key changes
- 768799·Surya P Bhatt Richard Casaburi Alvar Agusti et Al. Chronic obstructive pulmonary disease: hiding in plain sight, a Statement from the COPD Foundation Medical and Scientific Advisory Committee
- 769092·Leonardo M Fabbri et al. COPD and multimorbidity: recognising and addressing a syndemic occurrence
Estudios
- 759397·Alberto Sandiumenge et Al.-Systemic Inflammation Differences in Brain-vs. Circulatory-Dead Donors: Impact on Lung Transplant Recipients
- 759578·Alberto Papi et Al.-Relationships between symptoms and lung function in asthma and/or chronic obstructive pulmonary disease in a real-life setting: the NOVEL observational longiTudinal studY
- 759689·Kilian Vellvé et Alt.- Pulmonary vascular reactivity in growth restricted fetuses using computational modelling and machine learning analysis of fetal Doppler waveforms.
- 769273· Singh D, Criner GJ, Agustí A et al. Benralizumab Prevents Recurrent Exacerbations in Patients with Chronic Obstructive Pulmonary Disease: A Post Hoc Analysis
- 769685·Nuria Olvera et Al.- Lung Tissue Multi-Layer Network Analysis Uncovers the Molecular Heterogeneity of COPD
Imagen creada con imágenes de infografía de la noticia original.
